3D printing's come a long way.
The technology has definitely gone mainstream, now that hobbyists can buy inexpensive devices online and companies are experimenting with everything from food to fashion to cars and housing. But it’s within healthcare that it has the biggest life-changing potential.

Abbott scientists and engineers use 3D printing to develop prototype tools that enhance product development for devices used to treat vascular disease. They prototype parts used in next-generation medical diagnostics.
In fact, these 3D-printed items could make it faster, more innovative, less expensive and more efficient to develop new medical devices and products—all with the ultimate goal of helping people live longer, healthier lives. At a time when personalized and customizable medicine is taking center stage, 3D printing technology today points to increasingly sophisticated uses tomorrow.
3D printing—or "additive manufacturing," as it's sometimes called—converts a digital CAD (computer aided design) file into a three-dimensional structure by laying down layer after layer of thin material such as resin or plastic, which is often cured with ultraviolet light.
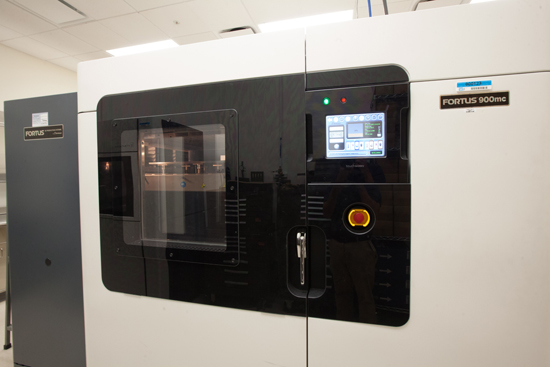
3D printer housed in Abbott’s diagnostics business in Santa Clara, California.
Moving Faster By Leveraging Learnings Across Abbott
Earlier this year, Abbott's Scientific Governing Board—made up of senior scientific leaders from across the company’s different focus areas—launched a 3D Task Force headed by John Capek, executive vice president, Ventures, and Jamey Jacobs, divisional vice president of global product development for Abbott’s vascular business.
The 3D Task Force's mission? "To identify and leverage best practices and learnings from around Abbott, helping everyone to move faster and smarter," and, said Jacobs, "to discover where can we find the cutting edge of 3D capabilities outside Abbott that could provide technically advanced solutions."
With just a CAD file, a physical piece takes shape "directly from the engineer's design file without requiring a machinist to translate the drawings into a prototype using traditional machine shop tools—something that would take days or weeks," Jacobs added. "You can get complex, quick working models and fail or succeed fast. It also allows new solutions because you can 3D-print something that couldn’t possibly be machined. It can truly revolutionize our design capabilities."
Working across Abbott’s different medical device businesses—including those focused on vascular, diabetes and diagnostics—is paying off, said Senior Volwiler Research Fellow Syed Hossainy, who leads the 3D printing initiative within Abbott's vascular division. Brainstorms with colleagues from the diabetes care businesses about the challenges in their fields led to 3D-printing breakthrough ideas.
In addition to working with each other, Capek challenged the businesses to partner with emerging external resources—start-up firms and forward-thinking organizations—that are pushing innovation in the 3D space, especially when it comes to patient-specific advances. In fact, Abbott's vascular R&D team recently worked with the Wake Forest Institute for Regenerative Medicine’s Dr. Anthony Atala, one of the world's leading regenerative medicine researchers, to prototype a 3D-printed bioabsorbable heart support device that's customized for a patient's own anatomy and function. "In the future," said Hossainy, "a device like this has real potential to benefit people with advanced congestive heart failure."
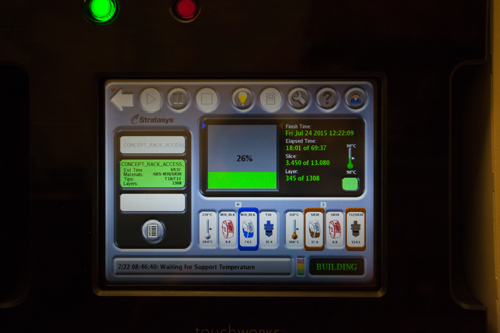
3D printer at Abbott’s diagnostics business in Santa Clara, California.
Bringing 3D-Printed Devices to Life, for Life
Among the ways this technology’s taking shape at Abbott:
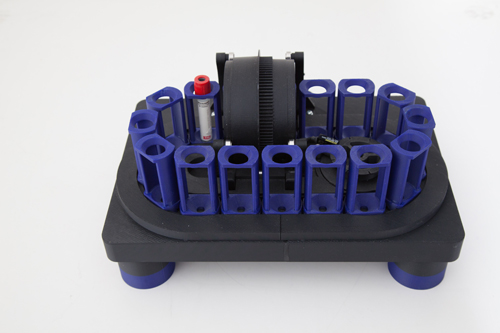
3D-printed prototype of a patented hematology analyzer, which runs automated tests on blood samples. This device allowed engineers from Abbott’s diagnostics business to model parts of the assembly and test the concept before production.
IMPORTANT SAFETY INFORMATION
SUPERA™ PERIPHERAL STENT SYSTEM
INDICATIONS:
The Supera™ Peripheral Stent System is indicated to improve luminal diameter in the treatment of patients with symptomatic de novo or restenotic native lesions or occlusions of the superficial femoral artery (SFA) and/or proximal popliteal artery with reference vessel diameters of 4.0 to 6.5 mm, and lesion lengths up to 140 mm.
CONTRAINDICATIONS:
The Supera™ Peripheral Stent System is contraindicated in:
patients who are judged to have a lesion that prevents complete inflation of an angioplasty balloon or proper placement of the stent or stent delivery system
patients who cannot receive antiplatelet or anticoagulation therapy. Based on in vivo thrombogenicity testing, the device should not be used in patients who cannot be anticoagulated as there may be some thrombus formation in the absence of anticoagulation.
WARNINGS:
This device is intended for single-use only. Do not reuse. Do not resterilize. Do not use if the package is opened or damaged.
Use this device prior to the “Use By” date as specified on the device package label. Store in a dry, dark, cool place.
DO NOT use if it is suspected that the sterility of the device has been compromised.
Persons with known hypersensitivities to Nitinol and / or its components (e.g. nickel titanium) may suffer an allergic reaction to this implant.
Administer appropriate antiplatelet therapy pre- and post-procedure.
Careful attention should be paid when sizing and deploying the stent to prevent stent elongation. In the SUPERB clinical study, stent elongation was associated with a decrease in patency at 12 months.
PRECAUTIONS:
The Supera™ Peripheral Stent System should only be used by physicians and medical personnel trained in vascular interventional techniques and trained on the use of this device.
The long-term safety and effectiveness of the Supera™ Peripheral Stent System has not been established beyond three years.
The safety and effectiveness of the Supera™ Peripheral Stent System has not been established in patients who:
are less than 18 years old
are pregnant or lactating
have in-stent restenosis of the target lesion
have known hypersensitivity to any component of the stent system (e.g., nickel)
cannot tolerate contrast media and cannot be pre-treated
have uncontrolled hypercoaguability and / or other coagulopathy
This device is not designed for use with contrast media injection systems or power injection systems.
The flexible design of the Supera™ Stent may result in variation in the deployed stent length.
Magnetic Resonance Imaging (MRI)
A patient with this device can be scanned safely only under specific conditions. Failure to follow the conditions may result in severe injury.
Non-clinical testing has demonstrated the Supera™ Stents are MR Conditional for lengths up to 250 mm. A patient with this stent can be scanned safely, immediately after placement, under the following conditions:
Static magnetic field of 1.5 or 3.0 Tesla
Highest spatial gradient magnetic field of 2,500 Gauss/cm or less
Maximum MR whole-body-averaged specific absorption rate (SAR) of
2 W/kg for landmarks (i.e. center of RF coil) above the umbilicus
1 W/kg for landmarks below the umbilicus and above the mid-thigh
0.5 W/kg for landmarks below the mid-thigh for 15 minutes of scanning (per pulse sequence), operating in the Normal Operating Mode (i.e., MR system mode of operation where there is no physiological stress to the patient). The legs of the patient should not be touching during the procedure.
POTENTIAL ADVERSE EVENTS:
Potential adverse events include, but are not limited to:
Abrupt closure
Allergic reaction (contrast medium; drug; stent material)
Amputation or limb loss
Aneurysm or pseudoaneurysm in vessel or at vascular access site
Angina or coronary ischemia
Arrhythmia (including premature beats, bradycardia, atrial or ventricular tachycardia, atrial or ventricular fibrillation)
Arteriovenous fistula
Bleeding complications requiring transfusion or surgical intervention
Death
Detachment of a system component or implantation in an unintended site
Embolization, arterial or other (e.g. air, tissue, plaque, thrombotic material, or stent)
Emergent surgery
Fever
Hematoma or hemorrhagic event, with or without surgical repair
Hyperperfusion syndrome
Hypertension / Hypotension
Infection
Myocardial infarction
Pain (leg, foot, and/or insertion site)
Partial stent deployment
Peripheral nerve injury
Pulmonary embolism
Renal failure or insufficiency
Restenosis of vessel in stented segment
Shock
Stent malapposition or migration, which may require emergency surgery to remove stent
Stent strut fracture
Thrombosis or occlusion
Stroke
Transient ischemic attack
Venous thromboembolism
Vessel dissection, perforation or rupture
Vessel spasm or recoil
Worsening claudication or rest pain
CAUTION:
This product is intended for use by or under the direction of a physician. Prior to use, reference the Instructions for Use, inside the product carton (when available) or at eifu.abbottvascular.com or at medical.abbott/manuals for more detailed information on Indications, Contraindications, Warnings, Precautions and Adverse Events.
Please be aware that the website you have requested is intended for the residents of a particular country or region, as noted on that site. As a result, the site may contain information on pharmaceuticals, medical devices and other products or uses of those products that are not approved in other countries or regions.
The website you have requested also may not be optimized for your specific screen size.
FOLLOW ABBOTT